

Vaccinated people have antibodies. People who've recovered from Covid-19 have antibodies. Whose antibodies are better? ...longer lasting? Should recovered people also get vaccinated, and if so, will they gain anything? Will society as a whole gain anything? How long does immunity last? What about the Delta variant and other mutations? You probably already have an opinion on all of the above, and maybe even think you know all of the answers. But the true answers might surprise you, and by reading further, it's likely you'll take home new knowledge and reasonable expectations about the protection offered by both vaccination and natural immunity. We're going to use science only, specifically a thorough review of the major, real-world scientific studies, to discover the answers to these questions... no CNN, no FOX, no media articles, no TV, no Youtube videos, no alternative press, and no opinions, expert or otherwise, by politicians, media talking heads, or public health officials. Only published or posted scientific studies. We've conducted an in-depth review of the major relevant scientific studies, have read and analyzed the studies themselves, and present here for your review and interpretation, the results. We'll discuss the results below and come up with answers, taken from the studies, to what will likely be your major questions. Finally, we'll summarize and review the sixteen studies themselves. Why the emphasis on science, and not emotion, religion, politics, or economics, to name a few alternatives? Because the people in charge say they're setting public health policy according to what "the science" dictates. Let's see if that is indeed the case.
The results here are presented in levels. If you want a basic understanding (Level 1) but aren't fond of words, take a look at the first picture below, where results from 8 out of 16 of these studies are presented in an easy-to-read graph. To gain a Level 2 understanding, read through the "Questions & Answers" section, which presents major findings, results, conclusions, and analyses from the studies in a simple Q&A format. To advance to Level 3, read the remainder of this research survey which summarizes and discusses every one of the sixteen studies. To gain an even deeper understanding (Level 4), read the scientific studies themselves. (Links to all studies are included below.) Finally, to advance to Level 5, do your own research. Read additional studies related to the topic at hand...not media articles or statements by governmental organizations but actual scientific studies...and if you find a good related study, please bring it to our attention in the comments below. We encourage you to dig deep, educate yourself, and try to educate those around you to the greatest extent possible.
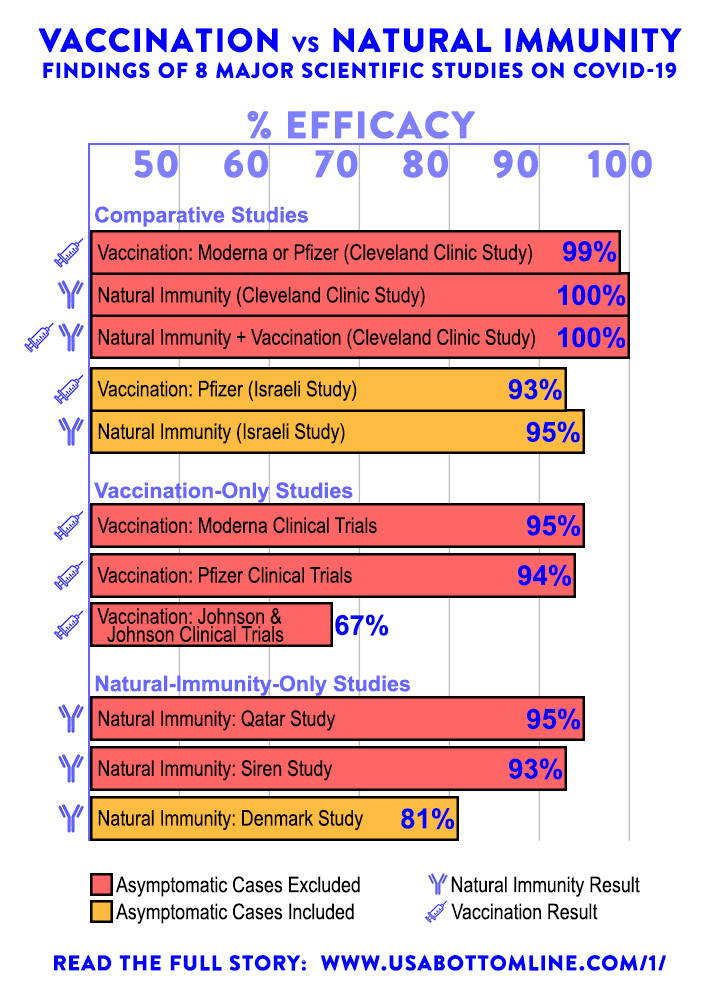
In deciding which participants had contracted Covid-19, some studies included only symptomatic cases, meaning a participant had to test positive for Covid-19 and had to show symptoms of Covid-19 before they were considered to have contracted it. This is the norm, the standard set by vaccine makers in their studies, so we have adopted it whenever a study reports multiple results. Other studies included asymptomatic cases, meaning a participant only had to test positive. One study [Siren Study #4] reported both symptomatic and asymptomatic cases and showed that including asymptomatic cases lowered the efficacy of both vaccines and natural infection by 9 to 10 percentage points. So to make a ballpark comparison between symptomatic and asymptomatic studies, you'll need to add a few percentage points to asymptomatic studies, or subtract a few percentage points from symptomatic studies.
When comparing results across studies, note that differences in study environments and methodology — the precise details of how researchers conducted each study — can swing the results by several percentage points in either direction. One such detail is testing methodology. Some studies used PCR testing only (the most common Covid-19 test) which is subject to false positives, false negatives, and other limitations. Other studies required genetic confirmation of Covid-19 sample positivity or even blood tests. With PCR-only studies, the quality/reliability of the specific test used, the skill level of the people administering/interpreting the tests, and the time period in which the tests were conducted can all influence the results. So when comparing across studies, be careful not to conclude anything based on a few percentage points difference. For example, you can't conclude that the Moderna vaccine is better than the Pfizer vaccine based upon the 1% difference in their clinical trials. However, you can safely conclude, by looking across studies, that the Moderna and Pfizer Vaccines and Natural Immunity are all three far superior to the Johnson & Johnson Vaccine. Speaking of the Johnson & Johnson Vaccine, it would have scored higher in efficacy, likely above 70%, if its clinical trials had been conducted using the same methods as the clinical trials for the Moderna & Pfizer Vaccines, testing against one instead of three virus variants, and excluding people with prior Covid-19 infection from participation. (See Studies #1, #2, and #3 below.)
Example — The Denmark Study [#8] included asymptomatic cases in their results and utilized PCR testing only. To make a ballpark comparison to symptomatic studies, use results from the similar Siren Study [#4] to add 9% to the Denmark Study, which gets you in the 90% range. Excluding false positives would also improve efficacy. The Denmark study did not include vaccinated people, so there's no vaccinated reference group for comparison. From the Denmark study, you can conclude that the efficacy of natural immunity is roughly comparable to the efficacy of mRNA vaccines. But you can't conclude that one is better than the other.
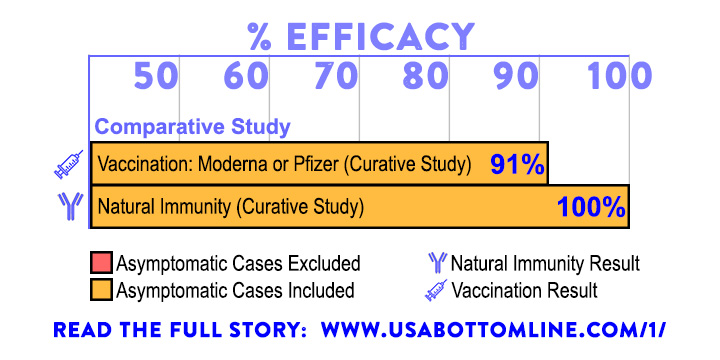
Comparative studies, on the other hand, test multiple drugs/treatments using the exact same experimental conditions. As long as the sample size is large enough (statistical significance), you can draw conclusions based on a few percentage points difference. The Cleveland Clinic [#5], Curative [#7], Israeli [#15], and Delta [#16] studies are examples of comparative studies, directly comparing mRNA vaccines and natural immunity. The Siren Study [#4] also provides comparative data between vaccination and natural immunity.
This survey of research addresses efficacy only. It addresses neither the safety of vaccination nor the safety of natural infection as immunization strategies. Both topics are beyond the scope of this survey. Nothing herein should be construed as medical advice. Consult a medical practitioner you trust if you want medical advice tailored to your individual situation.
1. Which provides better protection against Covid-19, Natural Immunity or Vaccination? Natural Immunity. Looking at the results across all studies, Natural Immunity provides the best protection, mRNA vaccines (Moderna & Pfizer) are a close second, and traditional vaccines (Johnson & Johnson and the rest) are a distant third. The 2-dose mRNA vaccines (by Moderna & Pfizer) are highly effective in preventing symptomatic Covid-19. Natural Immunity is comparable in efficacy, even slightly superior in efficacy, to the 2-dose mRNA vaccines, all scoring in the 90's percentage-wise. Other vaccines being utilized worldwide (including Johnson & Johnson, AstraZeneca, and CoronaVac) have moderate efficacy somewhere in the 60's percentage-wise; we call these "traditional vaccines" because they're developed using inactivated virus. Both Natural Immunity and the mRNA Vaccines are far superior to Traditional Vaccines. When the three USA-approved vaccines are taken as a whole, or when all worldwide approved vaccines are taken as a whole, natural immunity scores significantly better than vaccination in efficacy against Covid-19.
2. What is "Natural Immunity"? People who've had Covid-19 and recovered develop long-lasting antibodies and immune memory that protect them against future infection by the SARS-CoV-2 virus that causes Covid-19. We're looking at how effective this protection is in comparison to the protection provided by vaccine-induced immunity. Natural immunity is often called "natural infection" in the scientific studies.
3. How long do antibodies from natural immunity last? At least one year. Best guess: 2-4 years. In the early days of Covid-19, nobody knew the answer to this question. Not enough time had elapsed to test for the presence of antibodies one, two, and three years later. Today, about a year-and-a-half from the first reported cases of Covid-19, we know a lot more about year one. And we can make educated guesses about future years. The Korean Study [#10] shows that for naturally infected people, antibodies last at least a year. After one year, over 94% of participants had detectable antibodies against Covid-19, using only commercially available antibody tests. So Covid-19 antibodies last at least a year. Will they last 2 years? ...3 years? ...forever? We know that Covid-19 is not like seasonal flu, where antibodies last a few months, and it's not like measles, where antibodies last a lifetime. It's more like SARS or MERS. So the best educated guess is that Covid-19 antibodies last 2-3 years or longer, depending on the individual. This guess is based on the similarity between SARS-CoV-2 (virus causing Covid-19) and SARS-CoV-1 (the SARS virus from 2003) and MERS-CoV (the MERS virus from 2012). "In case of SARS-CoV-1, 90% and 50% of patients have been shown to maintain IgG antibodies for two and three years, respectively." [Korean Study #10] By extension, 50% of patients will maintain these antibodies for at least part of the 4th year. "The closely related viruses SARS-CoV and MERS-CoV induced immunity that typically lasted 2-3 years after infection." [Denmark Study #8]
But you're asking the wrong question. What you'd really like to know is "How long does natural immunity last?" Perhaps a lifetime. Focusing exclusively on bloodstream-circulating antibodies misses the big picture. Immune system defenses also include memory T cells and B cells as well as mucosal immunity. Studies #9 [La Jolla Institute for Immunology] and #11 [Washington University School of Medicine] dig deeper, testing bone marrow samples as well as blood samples, and looking at the four different types of immune memory. These studies conclude that immunity from natural infection is indeed long lasting. Even when antibodies are no longer detectable in blood samples, long lasting immune memory cells are likely present in the bone marrow of recovered individuals. For SARS-CoV-1, it's been demonstrated "that patients who recovered from SARS possess long-lasting memory T cells that are reactive to the N protein of SARS-CoV 17 years after the outbreak of SARS in 2003."
A related question is: How long does vaccine-induced immunity last? Since Covid-19 vaccines are relatively new, it's too early to tell. Currently available follow-up studies show that vaccine-induced antibodies are still present after several months. Looking at past vaccines and diseases, "it is unknown whether vaccine-induced immunity is as long-lived as that induced by natural infection."
Reality Check — Note that possessing immunity is not the same as being impervious to a pathogen. It does not absolutely guarantee that you won't get infected by that pathogen or that you won't get sick. That would be an unreasonable expectation. Immunity simply means that your body possesses the tools it needs to quickly fight off future infections.
4. Will naturally immune people gain additional benefit through vaccination? No. Not with the currently available vaccines. "Individuals who have had SARS-CoV-2 infection are unlikely to benefit from COVID-19 vaccination.... It is reasonable to expect that immunity acquired by natural infection provides effective protection against future infection with SARS-CoV-2. Observational studies have indeed found very low rates of reinfection over the following months among survivors of Covid-19. Reports of true reinfections are extremely rare in the absence of emergence of new variants. When such reinfections occur, it would be purely speculative to suggest that a vaccine might have prevented them.... This study provides direct evidence that vaccination with the best available vaccines does not provide additional protection in previously infected individuals.... A practical and useful message would be to consider symptomatic COVID-19 to be as good as having received a vaccine, and that people who have had COVID-19 confirmed by a reliable laboratory test do not need the vaccine." [Cleveland Clinic Study #5]
There have been a number of studies on hybrid immunity, i.e. the combination of vaccination and natural infection, with researchers raving about the robust response of antibodies in hybridly immune individuals. However, these are all serological studies, theoretical studies conducted on test tubes full of blood serum. Currently, the only real-world studies on this topic are the Cleveland Clinic Study #5, the CDC Kentucky Study #14, and the Delta Study #16. The additional benefit shown by these real-world studies ranges from none to slight.
5. What is "Efficacy"? It's a percentage reduction in risk achieved by a treatment, when compared to a control group. In our case, a control group is a group of people with no protection against the virus. The control group has not been vaccinated and they have not been previously infected. In a study, if 50% of a control group gets sick with the virus, but only 25% of the vaccinated group gets sick with the virus, that vaccine has an efficacy of 50%, because it has cut the risk of getting sick with the virus in half. In other words, the vaccine has reduced the risk by 50%. (See Pfizer Vaccine Study #1 for a more complex example of calculating efficacy.)
6. Should naturally immune people get vaccinated so that they won't spread the virus? No. There's no scientific evidence to support such a recommendation. Since vaccination provides no additional benefit to naturally immune individuals in preventing reinfection, it's highly unlikely to provide any additional benefit in limiting the spread. With the wide variety of vaccines on the world market that vary greatly in efficacy, we should be more worried about vaccinated people spreading the virus than we should about naturally immune people spreading the virus. In fact, if we use the likelihood of breakthrough infection, including asymptomatic reinfection, as a measure of a group's ability to spread the virus, vaccinated people are more likely to spread the virus than naturally immune people (see graph below).
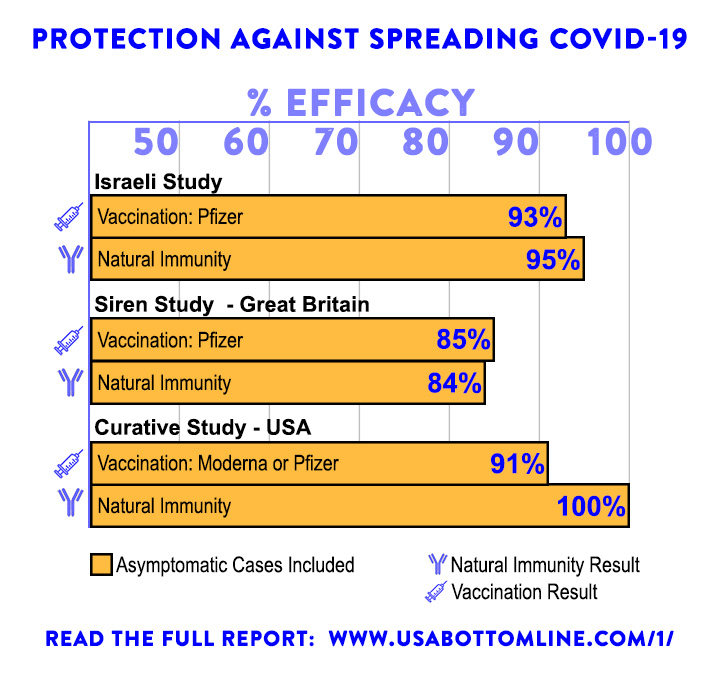
The graph above tells us that if we put vaccinated people into one group — everyone who's been fully vaccinated using the best available Covid-19 vaccines, and we put all recovered people into another group — everyone who's ever tested positive for Covid-19 and recovered, neither group would be more likely than the other to spread the virus. But not all vaccinated people have been fully vaccinated with the best available vaccines. Therefore, vaccinated people are more likely to spread the virus than naturally immune people. The graph above is based on Studies #4, #7, and #15. Study #16, entirely based upon the Delta variant, shows that vaccinated people are six times as likely as naturally immune people to experience a symptomatic or asymptomatic breakthrough infection, making them also more likely to spread the virus.
7. Will naturally immune people gain additional protection against Delta and other variants through vaccination? No. Not with the currently available vaccines that were all formulated based on the original Wuhan strain. In addition, recently infected individuals were likely infected by the Delta variant, giving them the best available protection against the Delta variant. "It is necessary to emphasize that these findings are based on the prevailing assortment of virus variants in the community during the study. It is not known how well these results will hold if or when some of the newer variants of concern become prominent. However, if prior infection does not afford protection against some of the newer variants of concern, there is little reason to suppose that the currently available vaccines would either. Vaccine breakthrough infections with variants have indeed been reported." [Cleveland Clinic Study #5]
8. Is there any harm done if naturally immune people get vaccinated? Yes. Currently, there's a worldwide shortage of vaccine. Valuable doses of vaccine should not be wasted on people who already have immunity. In addition, every medical intervention carries a possibility of adverse reaction, so it's wise to avoid unnecessary medical intervention.
Caution — Anyone who decides to get vaccinated after recovering from Covid-19 should do their research first. There's a mandatory minimum waiting period that varies from country to country, typically ranging from three months to six months. In addition, vaccination protocol for recovered people varies from country to country. In Israel, for example, a single dose of Pfizer Vaccine is given rather than two doses. [Delta Study #16]
9. How does the Delta variant change things? Not much. Vaccines drop 5-7% in efficacy but still provide strong protection [Public Health England Study #13]. Natural Immunity, likewise, drops a few percentage points in efficacy but still provides strong protection against Delta. Not surprisingly, those who were infected in 2021 have slightly stronger protection against Delta than those who were infected in 2020 [Thai Study #12]. This is presumably because the 2021 people were more likely to have been infected by the Delta variant.
But didn't Israel say that the vaccine wasn't working well? It was over the news. There's nothing in the scientific literature about this, only the following pronouncement by the Israeli Ministry of Health on July 5th 2021: "It is evident that since June 6th there was marked decline in the effectiveness of the [Pfizer] vaccine in preventing infection (64%) and symptomatic illness (64%). This decline has been observed simultaneously with the spread of the Delta variant in Israel. Nevertheless, the vaccine maintains an effectiveness rate of about 93% in preventing serious illness and hospitalization cases." Unfortunately, we can't apply any scientific scrutiny to their pronouncement, because no data and no published scientific study is available, only this one paragraph.
Why shouldn't we just take their word for it? Because that's not how science works, and the studies produced by national and international health agencies are often notoriously bad, incomplete, and/or politically motivated. (See CDC Kentucky Study #14 for one example.) Until if and when they publish their full report, or until separate studies confirm their results, the best course of action is to disregard this pronouncement. Basic unanswered questions include: What control group was used? How many people were included? What time period was studied? What methodology was used? And why did the reported results change from the 30% range to the 60% range in a matter of days? Did they include previously infected people in their study? If so, that one factor alone could dramatically lower efficacy.
In fact, an actual scientific study [Delta Study #16] conducted in Israel during the same time period did not utilize an unvaccinated control group at all, presumably because of a shortage of unvaccinated and not previously infected people in the general population. The Delta Study instead compared vaccinated people with previously infected people, and found that previously infected people had far superior protection against the Delta variant.
10. I'm vaccinated or naturally immune. Should I get a booster shot? It depends. Currently available boosters, all formulated based on the original Wuhan strain, are unlikely to provide additional protection, unless a) you're upgrading from an inferior vaccine to an mRNA vaccine or b) you have a deficient immune system. If a booster were to be formulated today based on the Delta variant, it would provide limited additional protection (around 6% gain in efficacy). As we move into the future, take into account at least these four things before making your decision: a) Have new variants arisen that have made the old vaccines ineffective? If so, they've likely also made natural infection by the old variants ineffective. b) How long has it been since your last shot of vaccine, or your last exposure to the virus? c) Has Covid-19 disappeared? d) What's your individual health situation? Medical advice must be tailored to each individual by their medical practitioners, and what works for the vast majority of people might not work for you, especially if you have a weak or compromised immune system. There's a good article just published in The Lancet that weighs the pros and cons of booster shots, not just on an individual level, but on a population-wide level. This article considers and cites many of the relevant scientific studies on the topic. For further reading, refer to the article "Considerations in boosting COVID-19 vaccine immune responses".
11. I'm vaccinated or naturally immune, but had a breakthrough infection. Should I get a booster shot? You already did. The breakthrough infection WAS your booster shot, and in all likelihood, you were immunized by and against the latest & greatest variant, currently Delta.
12. Should I go out and get infected on purpose to gain natural immunity? We can't recommend that. But if you're one of the few who still hasn't had the virus nor the vaccine, you might consider getting an antibody test, especially if you suspect that you might have had Covid-19. Most people who've had Covid-19 were never tested, so an antibody test will confirm whether you have any detectable immunity. If your test comes back negative, your options are to get vaccinated (for those fortunate enough to have access to vaccines) or to take your chances with the virus. For those who've already had Covid-19 or who've already been vaccinated, there's good evidence that the best way to maintain and improve that immunity is to return to your prepandemic life and not be afraid of any subsequent exposure to the virus. The Qatar Study [#6] noted a "strengthening of protective immunity due to repeated exposures that did not lead to established infection." Also see the following article from the MDPI Viruses journal which contains links to over 80 more scientific studies on the topic: Repeated Exposure to Subinfectious Doses of SARS-CoV-2 May Promote T Cell Immunity and Protection against Severe COVID-19
13. Are asymptomatic people considered infected? Do they have natural immunity? Not in most studies, and we don't know. The standard set by most scientific studies, including those conducted by the vaccine makers, is "no symptoms, no disease". Someone who merely tests positive for Covid-19 is not considered infected unless they also have confirming symptoms or confirming lab tests. This standard has the benefit of eliminating most false positives. It also focuses on the most important aspect, that of preventing disease. Asymptomatic breakthrough infections and mildly symptomatic breakthrough infections are to be expected in both vaccinated and naturally immune people, and are not indicative of a failure of the vaccine or natural immunity; rather they're indicative of the vaccine or natural immunity doing its job. In most studies presented here, asymptomatic "infections" do not count against the efficacy of either vaccines or natural immunity. A person who merely has a positive PCR test, without confirming symptoms, should not be considered naturally infected. There's a good possibility of a false positive or even a superficial detection of virus that never became systemic enough to trigger a lasting immune response. It's unknown at this point whether truly asymptomatic people have any natural immunity, so the safest bet is to presume no and to get an antibody test for confirmation. Mildly symptomatic people, on the other hand, do have lasting immunity as shown by the studies.
Practical Side Note — Preventing asymptomatic Covid-19 infection has never been considered a practical goal. As mentioned above, the standard set by most scientific studies and followed by the vaccine makers themselves in their clinical trials is "no symptoms, no disease". The goal is to prevent symptomatic infections, hospitalizations, and deaths. In that regard, both vaccines and natural immunity are highly effective against all known variants.
14. Why study natural immunity? Because natural immunity will be the major driving force in ending the pandemic, and because most of the lessons we learn about natural immunity should also apply, to a large extent, to vaccine-induced immunity. If most of the world were to eventually get vaccinated, natural immunity will still be the force that ends the pandemic by immunizing populations after breakthrough infections.
15. Will "Herd Immunity" ever be reached? Probably, and soon in the USA. Herd immunity is resistance of a population to an infectious disease by virtue of a sufficient percentage of the population acquiring immunity. We've seen that individuals acquire a level of immunity to Covid-19 through either vaccination or natural infection. So the first thing to calculate is the percentage of the population that has some immunity. In the USA, as of 9/13/2021, nearly 210 million people (63.2% of the population) had received at least one dose of vaccine acquiring some level of immunity [Source: CDC Covid-19 Vaccine Tracker]. As of 9/8/2021, over 40.5 million cases of Covid-19 had been reported [Source: CDC Covid-19 Data Tracker]. Because not everyone gets tested and because many people who get Covid-19 don't know they've had it, the number of actual cases of Covid-19 is estimated to be a multiple of the number of confirmed cases.
While the exact number of Covid-19 cases can't be known, it's estimated to be anywhere from 2x to 5x the number of confirmed cases, depending on who does the estimation. The most conservative estimate of 2x would give the USA a case count of 81 million; 3x, 122 million; 4x, 162 million; and 5x, 203 million. But we can't simply add the vaccinated numbers and the infected numbers because there's overlap. Many people were both vaccinated and infected. Let's assume that people who've had Covid-19 are no more or less likely to get vaccinated than those who haven't. This is a reasonable conservative (underestimating) assumption since most people who've had Covid-19 never got tested, some people got infected after vaccination, and the US has been urging previously infected people to get vaccinated nevertheless. So an estimate of 2x would add 30 million additional people to the immune population and an estimate of 5x would add 75 million. With an overall population of 333 million, the percentage with immunity ranges from 72% to 86%. Taking the midpoint gives us a rough estimate of 79% of the US population that currently has immunity. This is near or above the threshold at which herd immunity is said to kick in. One fact that adds to herd immunity is that children are included in the population and children are far less susceptible to Covid-19 than adults. One fact that hurts herd immunity is that Covid-19 protection in the immune is not 100%, especially in those partially vaccinated or who received the Johnson & Johnson vaccine.
So herd immunity is likely near in the USA. Signs that herd immunity has commenced will be a decrease in hospitalizations and deaths. Another sign will be that the percentage of hospitalized Covid-19 patients that are vaccinated will start to go up as the virus runs out of unvaccinated first-timers to infect. We see some evidence of this already in US news reports that initially were stating that 1% of hospitalizations were vaccinated and now are stating that 15% of hospitalizations are vaccinated. Recent reports out of Israel, a country with a much higher vaccination percentage than the USA, are stating that 60% of Covid-19 hospitalizations are vaccinated.
16. Are "Vaccine Passports" or mandates effective? Are better options available? No and yes. Vaccine passports are extremely unlikely to be effective in controlling virus spread, they exclude people with superior immunity, and better options are available. If the goal is to maximize profits for the pharmaceutical companies, then yes, vaccine passports do exactly that. But if the goal is to maximally protect public health, there are better options, and we outline several of them below. If the Covid-19 vaccines were perfect, it would be a different story, but current vaccines have a real-world efficacy in the 60%-90% range. That means that 10%-40% of vaccinated people (depending on the vaccine they've taken) are subject to breakthrough infection and are potential spreaders of the virus. That percentage of vaccinated potential spreaders increases if you include asymptomatic spreaders. Lowering protection even further are current and future virus variants, medical and religious exemptions, the fact that some companies accept one dose of a 2-dose vaccine as proof of vaccination, and the fact that it's easy for people with no immunity to buy or print counterfeit vaccination certificates. It could easily happen that the majority of people admitted through a vaccine-passport system would be potential spreaders of the virus.
Not only do vaccine passports provide a false sense of security, but they exclude people with superior protection, the naturally immune. Any vaccine-passport system would be improved by accepting either a positive antibody test, a positive Covid-19 test (after a recovery period), or a recovery certificate from a doctor as being equivalent to proof of vaccination. This would increase the overall immunity level of the group admitted.
A second improvement to any passport system would be to add an expiration date, because we don't know how long immunity in vaccinated people will last. Should a 2-year-old or 3-year-old vaccination certificate be just as good a new one? Let's pick an expiration of one year as an example. A vaccination certificate would be good for one year from the date of last injection. A positive antibody test would also be good for one year from the date of test. After a year, a person could opt to either get a new antibody test or a booster shot, mix or match. Vaccinated people could opt to get an antibody test instead of a booster shot, and naturally immune people could opt to get a booster shot instead of an antibody test.
A third improvement to any passport system would be to weed out the inferior vaccines, the partially vaccinated, and those with no immunity. Two doses of either the Pfizer or Moderna vaccine would be required, or one dose of a traditional vaccine followed by a booster shot of mRNA vaccine. Positive antibody tests would also be accepted. Medical and religious exemptions would be eliminated, if allowed by law. This would produce the strongest possible vaccine-passport system. Still, somewhere in the range of 10%-20% of people admitted would be potential spreaders of the virus, and counterfeit certificates would remain a problem.
A simpler system could be implemented instead, an antibody-test-passport system, that would provide equivalent protection. This system would assure that everyone — the vaccinated and the naturally immune — still had detectable antibodies. An antibody-test-passport system would simply require a positive antibody test. A certificate would be good for a period of time (one year using our example above) from the date of the antibody test. There would be no more need to worry about which vaccine a person had taken.
The strongest system of all would be to exclude vaccinated people altogether and require proof of either natural immunity or hybrid immunity (see Delta Study #16). Implementation details, including specialized tests, would have to be worked out.
Currently, vaccine passports are being debated in the U.S. courts with regard to issues such as medical privacy, civil liberties, and public health. We've shown that better options are available. However, currently, under the best possible vaccine-passport system, somewhere in the range of 10%-20% of people admitted would be potential spreaders of the virus, and counterfeit certificates would remain a problem. That 10%-20% estimate would increase should new virus variants emerge that render the old vaccines less effective. In the past, vaccine mandates have been effective only against stationary targets such as Measles, Mumps, Rubella, Diphtheria, Tetanus, Whooping Cough, Polio, and Smallpox. Moving targets, such as the seasonal flu, have not had vaccine mandates for practicality reasons: in the years it would take to inoculate the whole world, the virus would have mutated or disappeared.
As the percentage of the population grows who were either vaccinated against or previously infected by Covid-19, and given the questionable effectiveness of the best-possible passport system, we must ask whether the vaccine-passport idea itself is an exercise in futility. Is there a better option? Is there a best option? Perhaps. We'll call that option "Return to Normal" and it should be given serious scientific consideration. The "Return to Normal" system is far easier than all other systems to implement because it requires no implementation. It doesn't discriminate and it doesn't violate anyone's privacy or civil liberties. But is it in the best interest of public health? Time will tell.
What is the "Return to Normal" system and what scientific evidence backs it? "Return to Normal" means precisely what it says: get rid of all Covid-19-related lockdowns, closures, vaccination mandates, mask mandates, social distancing, and other restrictions. Go back to the way things were pre-Covid-19, and encourage both vaccinated and naturally immune people to return to normal and circulate and interact with others as widely as they used to do. It's well known that the first case of Covid-19, for an unvaccinated person, is potentially the most dangerous. While the vast majority of infected people show only mild to moderate symptoms, or no symptoms at all, a large number of people have experienced serious-to-critical illness or even death. On the other hand, it's rare for vaccinated and naturally immune people who test positive for Covid-19 to experience serious illness, and most such cases of breakthrough infection are mild if not asymptomatic.
In countries such as the USA, where everyone is currently either vaccinated, previously infected, refusing to get vaccinated, or a child, and the percentage of vaccinated + previously infected people approaches or exceeds a herd immunity threshold, it makes sense to implement a "Return to Normal" strategy and let the virus exhaust and extinguish itself by running out of infectable subjects, while at the same time allowing the population of vaccinated and naturally immune people to get back to normal and strengthen their immunity through repeated exposure to the virus. The Qatar Study [#6] noted a "strengthening of protective immunity due to repeated exposures that did not lead to established infection. Notably, a recent study from Qatar indicated an association between higher antibody titers and repeated exposures to the virus.... These findings are striking, as the epidemic in Qatar has been intense, with half of the population estimated to have acquired this infection at some point since its introduction into Qatar early in 2020. It is highly probable that a proportion of the population has been repeatedly exposed to SARS-CoV-2, but such re-exposures did not lead to more than a limited number of documentable reinfections. Other lines of evidence also support a low frequency of reinfection. The epidemic in Qatar grew rapidly and declined rapidly.... No second wave materialized in 2020 following the epidemic peak in May 2020, despite easing of public health restrictions." Currently, several US states have attempted a "Return to Normal" strategy, with backlash and nonparticipation by those who prefer lockdown, mitigation, and isolation strategies. We may have some good data, within a few months, on how well the various strategies have worked.
Temporary Nature — It deserves emphasis that the need for any sort of Covid-19 passport system or mandate disappears as soon as the virus diminishes or becomes endemic in the population.
17. Based on the studies, what advice can you give to public health officials? In particular, what should they be doing differently? Follow the science. Start recognizing natural immunity, because it will be the primary force in ending the pandemic. Stop lumping the naturally immune in with "the unvaccinated". Stop excluding and discriminating against the naturally immune. Stop wasting vaccine on the naturally immune. Give public health first priority, not profit for the pharmaceutical companies. Set practical goals: stopping asymptomatic spread, for example, is not a practical goal. Tell the truth and give people realistic expectations. Stop spreading unfounded fear, panic, and hysteria. For example, the vast majority of naturally immune and fully vaccinated people need not fear additional exposure to the virus. Start acting globally, not just nationally, because a pandemic's not over in one country until it's over in every country.
18. Why do some results here contradict the recommendations of the CDC, or US Government, or US media? There's no scientific explanation. When science is pitted against politics and money, politics and money often emerge victorious. A better question would be: "Why do the government's recommendations contradict the findings of the worldwide scientific community?" Specifically, we're talking about the CDC's recommendation that all people with previous Covid-19 infection get vaccinated nevertheless. While there are definite monetary/political motivations, are there also valid scientific motivations behind this recommendation? Let's first note that not all worldwide governments advocate for vaccination of recovered people. India, for example, has recommended the precise opposite, so that vaccine is not wasted on the already immune. The European Union allows people who've recently recovered from Covid-19 to obtain a vaccine "passport". So does Israel.
We searched for real-world scientific studies that might contain evidence of vaccination's superiority over natural immunity, and found none. What we found was a single study conducted by the CDC and frequently cited by the news media. The study is based on data out of Kentucky [CDC Kentucky Study #14]. The CDC Kentucky Study claims that naturally immune people can double their protection by also getting vaccinated, but it doesn't study the efficacy of vaccination on its own versus natural immunity on its own.
We also found a "fact-checking" article by USA Today that states "Based on our research, we rate FALSE the claim that if you have natural immunity from a bout of COVID-19, you don't need the vaccine." This serves as an example of the misinformation prevalent in the news media. It's only one example out of thousands of such news articles on the topic, and we don't intend to cover more than one of them. Since we're conducting a scientific survey, let's examine the science backing their "fact-checking". USA Today's "research" consists of gathering opinions from a handful of experts, along with citing the CDC Kentucky Study [#14] and a total of two other scientific studies. Expert opinion is not scientific evidence, so should be discounted and disregarded. As a practical matter, it's easy to find a few experts to state the desired opinion, or even a few thousand experts if you have the time, all opining in unison. Let's look at USA Today's three cited scientific studies instead. The first study is a theoretical investigation of the binding of natural- and vaccine-induced antibodies to virus. The study is interesting, but it's not a real-world study; the authors don't make any bold claims about what their results might mean in the real world; only the fact-checker makes those bold claims. The second study is irrelevant to the question at hand. It concludes that previously uninfected people have 5 times the risk of previously infected people, which tells us that natural immunity is effective, but it says nothing about vaccination; it was conducted entirely before the advent of vaccines. The third study is the CDC Kentucky Study [#14], which also says nothing about whether natural immunity is superior to vaccination or vice-versa, only that naturally immune people can double their protection by also getting vaccinated. It begs the question, "Can vaccinated people also double their protection by getting infected?" Before you get excited about doubling your protection, note that other studies we've reviewed such as the Cleveland Clinic Study [#5] show no additional benefit to vaccinating the naturally immune. In fact, the CDC Kentucky Study has fundamental flaws that invalidate its results. (See CDC Kentucky Study [#14] below for a detailed review.) The USA Today article does not present a single real-world scientific study that backs their fact-checking, and it conveniently ignores all of the massive real-world studies ([#4], [#5], [#6], [#7], [#8], [#15], [#16]) that would change their fact-checking result to TRUE. Sadly (for science that is), the CDC Kentucky Study also conveniently ignores all of the same massive real-world studies, not citing a single one of them.
In conclusion, the answer to this question can't be found in the scientific literature. Only very weak scientific evidence is presented by the CDC to back their chosen position. The media provides only weak scientific evidence too but mostly echoes the CDC. So we can only speculate about the real reason behind this complete denial of scientific evidence. One potential reason is convenience. As we've seen in Question #15 above, it's easy to track the number of vaccinated people. It's hard to track the number of naturally immune people. In addition to convenience, money and politics are the most likely culprits. $24 a dose, multiplied by 200 million doses, is $4.8 billion dollars. That's the USA's latest order of Pfizer Vaccine. A simple internet search shows a $20-$25 billion-a-year market for Covid-19 vaccines, with forecasts going all the way out to year 2030. Pharmaceutical companies would stand to lose a lot of money if the pandemic were to end prematurely.
19. If everyone had gotten vaccinated when they were first eligible, would this have stopped the emergence of Delta and other variants? No. The "If" part of this question is a mathematical impossibility. As of today, there's still a vaccine shortage, not nearly enough supply available to vaccinate the whole world. This naive question is also very US-centric and ignores the fact that the Delta variant arose in India where very little vaccine was available at the time the variant emerged. See Known Variants & Country of Origin appendix for more info.
20. What's the unique value in the real-world studies presented here? The studies are valuable because they've already been conducted and it'll become difficult-to-impossible to perform similar studies in the present-to-future. Most studies, including the vaccine-makers own studies, require a control group of unvaccinated, never-before-infected individuals, against which to measure efficacy. As the virus spreads and as most of the world gets vaccinated, individuals eligible for the control group will become increasingly rare. In fact, the most recent study included here, Delta Study #16, was unable to produce such a control group for comparison. Muddying the results will be people with multiple exposures in groups of both vaccinated and naturally immune individuals. In a vaccinated test group, it'll be difficult to judge whether a person's immunity is due to the vaccines they've taken or the exposures they may have had to the virus. Similarly, in a naturally immune test group, it'll be hard to isolate whether a person's immunity is due to a single exposure or due to multiple exposures to the virus.
STUDY #1: PFIZER VACCINE
"Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine"
Published 12/10/2020, New England Journal of Medicine
https://www.nejm.org/doi/full/10.1056/nejmoa2034577
This study details the Phase 3 clinical trials for the Pfizer-BioNTech Covid-19 vaccine (which we'll call "Pfizer Vaccine" for brevity). It took place predominantly in the USA at 130 sites with 22 more sites in 5 other countries. Completing the study were 18,508 participants in Group #1 who received two doses of the vaccine, and 18,435 participants in Group #2 who received two doses of a placebo. People excluded from the study: "Key exclusion criteria included a medical history of Covid-19, treatment with immunosuppressive therapy, or diagnosis with an immunocompromising condition." Follow-up duration: 50% of participants were tracked for two months and the other 50% were tracked for 14 weeks after completing injections. "There were 8 cases of Covid-19 with onset at least 7 days after the second dose among participants assigned to receive BNT162b2 and 162 cases among those assigned to placebo; BNT162b2 was 95% effective in preventing Covid-19". "These data do not address whether vaccination prevents asymptomatic infection", meaning participants were only tested for infection if they showed any symptoms. The study doesn't mention multiple strains of Covid-19, and given that it was conducted mostly in the USA over the given time period, it's likely that a single strain predominated.
Example — Want to know how they calculated efficacy? 8/18508 = .04322% infected in Group #1 (vaccine group). 162/18435 = .87876% infected in Group #2 (control/placebo group). Difference = .87876% - .04322% = .83554% . Efficacy = Difference / (Control Group Infection %) = .83554% / .87876% = 95.08% .
STUDY #2: MODERNA VACCINE
"Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine"
Published 12/30/2020, New England Journal of Medicine
https://www.nejm.org/doi/full/10.1056/nejmoa2035389
This study details the Phase 3 clinical trials for the Moderna Covid-19 vaccine, which took place entirely in the USA. Completing the study were 14,134 participants in Group #1 who received two doses of the vaccine, and 14,073 participants in Group #2 who received two doses of a placebo. "Eligible participants were persons 18 years of age or older with no known history of SARS-CoV-2 infection and with locations or circumstances that put them at an appreciable risk of SARS-CoV-2 infection, a high risk of severe Covid-19, or both." Follow-up duration: "As of November 25, 2020, the participants had a median follow-up duration of 63 days (range 0 to 97) after the second dose, with 62% of participants having more than 56 days of follow-up." "Symptomatic Covid-19 illness was confirmed in 185 participants in the placebo group and in 11 participants in the mRNA-1273 group; vaccine efficacy was 94.1%." "Severe Covid-19 occurred in 30 participants, with one fatality; all 30 were in the placebo group." Asymptomatic infections were not measured nor counted as infected. "This high apparent efficacy of mRNA-1273 is based on short-term data, and waning of efficacy over time has been demonstrated with other vaccines. Also, the efficacy of the vaccine was tested in a setting of national recommendations for masking and social distancing, which may have translated into lower levels of infectious inoculum."
STUDY #3: JOHNSON & JOHNSON VACCINE
"Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against Covid-19"
Published 4/21/2021, New England Journal of Medicine
https://www.nejm.org/doi/full/10.1056/NEJMoa2101544
This study details the Phase 3 clinical trials for the single-dose Johnson & Johnson vaccine (J&J Vaccine), one of three vaccines currently authorized for emergency use in the USA, the other two being the Pfizer Vaccine and the Moderna Vaccine. Compared to the clinical trials for the other two vaccines, the J&J Vaccine trial was conducted under more challenging circumstances, spread across nine countries, including two countries (South Africa & Brazil) where the Beta & Gamma strains predominated. The J&J Vaccine, like the Pfizer and Moderna Vaccines, was developed based on the original Wuhan virus strain. Unlike the other two vaccine studies, this one was conducted in environments containing three different strains. Group #1 consisted of 19,630 participants who received the vaccine and Group #2 consisted of 19,691 participants who received a placebo. Eligibility criteria was similar to the Pfizer & Moderna studies except that "participants were not excluded on the basis of SARS-CoV-2 infection or serostatus". "The median follow-up was 58 days (range 1 to 124), and 55% of participants had at least 8 weeks of follow-up." Vaccine efficacy came in at 66%-67% "against moderate to severe-critical Covid-19" and didn't change measurably if asymptomatic cases were included. "Vaccine efficacy was higher against severe-critical Covid-19 (76.7% for onset at =14 days and 85.4% for onset at =28 days)." (Best results are obtained by avoiding exposure for at least 28 days after vaccination.) "Vaccine efficacy against Covid-19 involving medical intervention ranged from 75% to 100%. Two cases of Covid-19 with onset at least 14 days after administration in the Ad26.COV2.S group and 29 such cases in the placebo group led to hospitalization. No hospitalizations for cases with an onset at least 28 days after administration occurred in the vaccine group, as compared with 16 hospitalizations in the placebo group.... Despite 86 of 91 cases in South Africa with sequenced virus having the 20H/501Y.V2 [Beta] variant, vaccine efficacy was 52% and 64% against moderate to severe-critical Covid-19 with onset at least 14 days and at least 28 days after administration, respectively, and efficacy against severe-critical Covid-19 was 73.1% and 81.7%, respectively.... Three deaths occurred in the vaccine group (none were Covid-19-related), and 16 in the placebo group (5 were Covid-19-related)."
STUDY #4: SIREN STUDY (ENGLAND)
"SARS-CoV-2 Infection Rates of Antibody-Positive Compared with Antibody-Negative Health-Care Workers in England: A Large, Multicentre, Prospective Cohort Study (SIREN)"
Published 4/9/2021, The Lancet
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00675-9/fulltext
This study examines whether individuals who have recovered from Covid-19 are protected from future reinfection, "whether antibodies against SARS-CoV-2 were associated with a decreased risk of symptomatic and asymptomatic reinfection". It also provides a comparison to a separate analysis they conducted evaluating the real-world efficacy of the Pfizer Vaccine. All Healthcare workers and hospital staff from publicly funded hospitals across the UK were eligible to participate. Group #1, the "Positive Cohort", consisted of 8,278 participants who tested antibody-positive upon enrollment or anytime prior to enrollment OR who tested antibody negative upon enrollment but had a positive PCR [Covid-19] test anytime prior to enrollment. Group #2, the "Negative Cohort", consisted of 17,383 people who were antibody negative upon enrollment and had no prior evidence of infection (evidenced by past PCR or antibody tests). Two strains of virus were common in the environment during the time of testing, the original Wuhan strain and the Alpha variant.
"The median length of follow-up per participant was 275 days (IQR 218-291) for the positive cohort and 195 days (131-214) for the negative cohort.... We have detected two probable reinfections and 153 possible reinfections in our positive cohort. 50 of the reinfections were symptomatic with typical COVID-19 symptoms, 28 with other symptoms, and 76 were asymptomatic. By contrast [in the negative cohort], we identified 1704 new PCR positive infections in patients, 1126 of whom had COVID-19 symptoms, 243 with other symptoms, and 293 were asymptomatic.... Using a COVID-19 symptomatic case definition aligned with positive PCR results, previous infection reduced the incidence of infection by at least 90% and even when we included all possible and probable reinfections reduced the incidence of reinfection by at least 84%. We believe this is the minimum probable effect...indicating some of these potential reinfections were probably residual RNA detection at low population prevalence rather than true reinfections.... Restricting reinfections to probable reinfections only, we estimated that...participants in the positive cohort had 99.8% lower risk of new infection than did participants in the negative cohort. Restricting infections to those who had COVID-19 symptoms, we estimated that participants in the positive cohort had a 93% lower incidence of new infection than did participants in the negative cohort.... Median protective effect [is] observed 7 months following primary infection. This time period is the minimum probable effect because seroconversions were not included. This study shows that previous infection with SARS-CoV-2 induces effective immunity to future infections in most individuals."
"The SARS-CoV-2 vaccination trials have typically investigated protection from symptomatic infection.... The BNT162b2 [Pfizer] vaccine phase 3 results reported 95% protection over 3 months of follow-up. Another phase 3 trial of the mRNA-1273 [Moderna] vaccine showed 94.1% efficacy against symptomatic (COVID-19 typical symptoms) SARS-CoV-2 infection, including severe illness, over a median of 2 months of follow-up. In a separate analysis on the SIREN cohort, we showed that the BNT162b2 [Pfizer] vaccine offered 70% protection from both symptomatic and asymptomatic infection, 21 days after the first dose, which increased to 85% 7 days after the second dose. Our findings of a 93% lower risk of COVID-19 symptomatic infection, after a longer period of follow-up, show equal or higher protection from natural infection, both for symptomatic and asymptomatic infection."
"After 7 months of follow-up, this large observational study showed that previous SARS-CoV-2 infection protects most individuals against reinfection for an average of 7 months. We have identified and investigated more potential reinfections than reported in the global literature to date, supporting the value of large prospective cohort studies such as SIREN. This study supports the hypothesis that primary infection with SARS-CoV-2 provides a high degree of immunity to repeat infection in the short to medium term; with similar levels of prevention of symptomatic infection as the new licensed vaccines for working-age adults. We have also shown that immunity from previous infection is protective against reinfection with the B.1.1.7 [Alpha] variant. Primary infection also reduces the risk of asymptomatic infection and thus onward transmission; this is particularly important as health care was considered a potential driver for ongoing community transmission during the first wave in the UK. Our findings increase the likelihood that this protection could also be attainable by vaccine-induced immunity, which a separate analysis on the SIREN cohort previously demonstrated."
STUDY #5: CLEVELAND CLINIC STUDY (USA)
"Necessity of COVID-19 vaccination in previously infected individuals"
Posted 6/19/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.06.01.21258176v3.full
This study included four groups, all four possible combinations of vaccinated and unvaccinated, recovered and never-infected individuals. "All employees of the Cleveland Clinic Health System, working in Ohio, on Dec 16, 2020, were screened for inclusion in the study." 12/16/2020 is the day Covid-19 vaccination was first available in the Clinic. Follow-up duration was 5 months. Group #1 consisted of 1359 recovered & unvaccinated employees; Group #2: 1220 recovered & vaccinated; Group #3: 20,804 unvaccinated with no prior infection; Group #4: 28,855 vaccinated with no prior infection. Vaccination was via either the 2-dose Moderna or Pfizer vaccines.
Motivation for Study: "Credible reports of previously infected persons getting COVID-19 are rare.... A strong case for vaccinating previously infected persons can be made if it can be shown that previously infected persons who are vaccinated have a lower incidence of COVID-19 than previously infected persons who did not receive the vaccine."
Results: "The cumulative incidence of SARS-CoV-2 infection remained almost zero among previously infected unvaccinated subjects, previously infected subjects who were vaccinated, and previously uninfected subjects who were vaccinated, compared with a steady increase in cumulative incidence among previously uninfected subjects who remained unvaccinated.... Of the 2154 SARS-CoV-2 infections during the study period, 2139 (99.3%) occurred among those not previously infected who remained unvaccinated or were waiting to get vaccinated, and 15 (0.7%) occurred among those not previously infected who were vaccinated. Not one of the 2579 previously infected subjects had a SARS-CoV-2 infection, including 1359 who remained unvaccinated throughout the duration of the study.... Conclusions: Individuals who have had SARS-CoV-2 infection are unlikely to benefit from COVID-19 vaccination, and vaccines can be safely prioritized to those who have not been infected before."
"This study was not specifically designed to determine the duration of protection afforded by natural infection, but for the previously infected subjects the median duration since prior infection was 143 days, and no one had SARS-CoV-2 infection over the following five months, suggesting that SARS-CoV-2 infection may provide protection against reinfection for 10 months or longer."
"It is reasonable to expect that immunity acquired by natural infection provides effective protection against future infection with SARS-CoV-2. Observational studies have indeed found very low rates of reinfection over the following months among survivors of COVID-19. Reports of true reinfections are extremely rare in the absence of emergence of new variants. When such reinfections occur, it would be purely speculative to suggest that a vaccine might have prevented them. Duration of protective immunity from natural infection is not known. However, the same also can be said about duration of protective immunity from vaccination. Uncertainty about the duration of protective immunity afforded by natural infection is not by itself a valid argument for vaccinating previously infected individuals. This study provides direct evidence that vaccination with the best available vaccines does not provide additional protection in previously infected individuals."
"Our study's findings have important implications. Worldwide, COVID-19 vaccines are still in short supply. As of May 17, 2021, only 17 countries had been able to reach ten percent or more of their populations with at least the first dose of vaccine. Given such a scarcity of the vaccine, and the knowledge that vaccine does not provide additional protection to those previously infected, it would make most sense to limit vaccine administration to those who have not previously had the infection. A practical and useful message would be to consider symptomatic COVID-19 to be as good as having received a vaccine, and that people who have had COVID-19 confirmed by a reliable laboratory test do not need the vaccine."
"The study follow-up duration was short, being only five months, but this was longer than published mRNA vaccine efficacy studies, and longer than the follow-up duration of the largest published vaccine effectiveness studies to date."
On children & the very elderly who were not included in this study of employees: "While one cannot generalize this study's findings to assume that prior infection would provide adequate immunity in these groups, there is also no reason to expect a vaccine to provide additional protection in these same groups."
"Lastly, it is necessary to emphasize that these findings are based on the prevailing assortment of virus variants in the community during the study. It is not known how well these results will hold if or when some of the newer variants of concern become prominent. However, if prior infection does not afford protection against some of the newer variants of concern, there is little reason to suppose that the currently available vaccines would either. Vaccine breakthrough infections with variants have indeed been reported."
STUDY #6: QATAR STUDY
"SARS-CoV-2 Antibody-Positivity Protects Against Reinfection for at Least Seven Months with 95% Efficacy"
Published 4/27/2021, The Lancet: EClinicalMedicine
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00141-3/fulltext
This is one of the largest studies that examines infection-induced immunity. It also has a lot to say about so-called "herd immunity" and the benefits of repeated exposure to the virus. It took place in the nation of Qatar, located in the Persian Gulf. The study followed two groups of people. Group #1 had 43,044 people who tested antibody-positive for Covid-19, meaning they had had a prior infection and recovered. Group #2 had 149,923 people who tested anti-body negative, meaning they had no detectable prior infection. None of the participants were vaccinated. The study was conducted by analyzing the national Covid-19 database of medical information, making every resident of Qatar a potential participant. "The database covers essentially all serological testing for SARS-CoV-2 conducted in Qatar, including both testing done on residual blood specimens collected for routine clinical care...and during a series of population-based serological surveys.... Individual time of follow-up ranged between 0 days and 34.6 weeks, with a median of 16.3 weeks.... Efficacy of natural infection against reinfection was estimated at 95.2%. Reinfections were less severe than primary infections. Only one reinfection was severe, two were moderate, and none were critical or fatal.... A large proportion of reinfections were minimally symptomatic (if not asymptomatic).... The cumulative risk of documented reinfection was rare, at ~2 per 1000 infected persons.... There was also no evidence that antibody-positive persons experienced any waning of protective immunity over time, as the incidence rate of reinfection versus month of follow-up did not show an increasing trend over seven months following the first antibody-positive test. To the contrary, there was a trend of decreasing incidence rate, possibly explained by the (very) slowly declining incidence rate in the wider population of Qatar during this study, or possibly by strengthening of protective immunity due to repeated exposures that did not lead to established infection. Notably, a recent study from Qatar indicated an association between higher antibody titers and repeated exposures to the virus."
On herd immunity — "These findings are striking, as the epidemic in Qatar has been intense, with half of the population estimated to have acquired this infection at some point since its introduction into Qatar early in 2020. It is highly probable that a proportion of the population has been repeatedly exposed to SARS-CoV-2, but such re-exposures did not lead to more than a limited number of documentable reinfections. Other lines of evidence also support a low frequency of reinfection. The epidemic in Qatar grew rapidly and declined rapidly, consistent with a susceptible-infected-recovered 'SIR' epidemic dynamic in which infection elicits strong immunity against reinfection. No second wave materialized in 2020 following the epidemic peak in May 2020, despite easing of public health restrictions."
STUDY #7: CURATIVE STUDY (USA)
"Incidence of Severe Acute Respiratory Syndrome Coronavirus-2 infection among previously infected or vaccinated employees"
Posted 7/8/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.07.03.21259976v2.full
This study was conducted by Curative Inc, a company that specializes in Covid-19 testing, on its own employees. They tested their employees daily for up to seven months. They used PCR tests exclusively to determine prior and subsequent infection, no antibody testing and no recording of symptoms. The sample size is smaller than comparable studies, but the daily testing frequency is unmatched by other studies. Group #1 consisted of 4313 unvaccinated participants with no prior infection; Group 2: 254 unvaccinated participants with prior infection; and Group #3: 739 vaccinated participants with no prior infection. Vaccinated participants received either the 2-dose Pfizer or Moderna vaccines. "During the observation period, 254, 0, and 4 SARS-CoV-2 incident infections were identified among Groups 1, 2, and 3, respectively.... Conclusion: We found a strong association between prior SARS-CoV-2 infection and vaccination for SARS-CoV-2 with either BNT162b2 or mRNA-1273 and the reduced incidence of SARS-CoV-2 when compared to those naive and unvaccinated to SARS-CoV-2. There was no difference in the incidence of SARS-CoV-2 between individuals who were vaccinated and individuals with prior SARS-CoV-2 infection." (Actually, there was a small difference, with the priorly infected faring significantly better than the vaccinated. See graph below.) "Combined with prior studies, our findings should provide increased confidence that those previously infected are at very low risk for repeat infection. Further research is needed to determine whether our results are consistent with the emergence of new SARS-CoV-2 variants."
STUDY #8: DENMARK STUDY
"Assessment of Protection Against Reinfection with SARS-CoV-2 Among 4 Million PCR-Tested Individuals in Denmark in 2020: A Population-Level Observational Study"
Published 3/17/2021, The Lancet
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00575-4/fulltext
This study compares population-level PCR test data gathered during Denmark's first Covid-19 surge (March to May 2020) with data gathered during the country's second surge (September to December 2020). "As part of Denmark's extensive, free-of-charge PCR-testing strategy, approximately 4 million individuals (69% of the population) underwent 10.6 million tests. Using these national PCR-test data from 2020, we estimated protection towards repeat infection with SARS-CoV-2.... Among eligible PCR-positive individuals from the first surge of the epidemic, 72 (0.65%) tested positive again during the second surge compared with 16,819 (3.27%) who tested negative during the first surge. Protection against repeat infection was 80.5%. The alternative cohort analysis [using tests throughout the year, not just the two surges] gave similar estimates.... We found no...evidence of waning protection over time (3-6 months of follow-up) vs =7 months of follow-up.... The closely related viruses SARS-CoV and MERS-CoV induced immunity that typically lasted 2-3 years after infection."
This study, like the Curative Study above, relied exclusively on PCR testing without further testing for false positives/negatives and without considering symptoms. Limitations: "Our dataset includes test results from people with few or no symptoms that might have resulted in a comparatively lower immune response than if we had only included individuals with moderate or severe symptoms. However, had we included only individuals with moderate or severe infections, our findings would then have been generalisable only to individuals with symptomatic infections. Also, misclassification of reinfections might have occurred if detectable virus RNA lingered for more than 3 months in some patients."
The Denmark Study shows that the efficacy of natural infection is comparable to the efficacy of available vaccines, but to a lesser degree than shown in the other studies. Why the difference? Because the Denmark Study included asymptomatic infections in their analysis, and most of the other studies didn't. The Siren Study [#4] showed that including asymptomatic cases would have dropped the efficacy of the Pfizer Vaccine down to roughly 85%. Reliance exclusively on PCR tests, which can yield false positives and negatives, is another limitation. The Cleveland Clinic Study [#5], in its review of prior comparable studies, had this to say about The Denmark Study: "The study did not compare vaccinated and unvaccinated people, and it is therefore an assumption to consider that a vaccine would have provided better protection in that particular population.... It is now well-known that a small number of people can continue to have positive PCR test results for several weeks to a few months after infection, one study finding that 5.3% remained positive at 90 days. It is possible that some of the positives picked up in the early part of the second surge were not necessarily new infections but residual virus from the tail end of the first surge. Since the actual number of infections was small, a few such misclassifications could change the rates substantially."
The Denmark Study did yield one potentially alarming result that could impact both vaccinated and naturally infected older adults. "In the alternative cohort analysis, among those aged 65 years and older, observed protection against repeat infection was 47.1%." A total of 31 reinfections were noted in this age group. How many were asymptomatic the first time? ...asymptomatic the second time? ...false positive the first time? ...false positive the second time? ...spurious detections of lingering virus RNA? ...cases of "long covid" where the patient hadn't recovered from the first infection? We don't know. A few misclassifications in a group of 31 would change the results dramatically. Before concluding that older adults, including vaccinated ones, have only moderate protection against breakthrough infection, we should look to other scientific studies for confirmation or contradiction. A larger-scale study [Israeli Study #15] found similar efficacy for natural infection across all age groups with only a 0%-3% decrease in efficacy for ages 80+. Likewise for vaccination, the Israeli Study found similar efficacy across all age groups with only a 1%-7% decrease for ages 80+.
STUDY #9: LA JOLLA INSTITUTE FOR IMMUNOLOGY STUDY (USA)
"Immunological Memory to SARS-CoV-2 Assessed for up to 8 Months After Infection"
Published 2/5/2021, Science
https://science.sciencemag.org/content/371/6529/eabf4063.long
This study examines how long natural immunity lasts, by analyzing "254 samples from 188 COVID-19 cases, including 43 samples at 6 to 8 months after infection". This study was conducted by the La Jolla Institute for Immunology and was funded by the NIH (National Institutes of Health) of the U.S. Government, National Cancer Society, and 10 other organizations. "This is the largest antigen-specific study to date of the four major types of immune memory for any viral infection.... Conclusion: Substantial immune memory is generated after COVID-19, involving all four major types of immune memory. About 95% of subjects retained immune memory at ~6 months after infection. Circulating antibody titers were not predictive of T cell memory. Thus, simple serological tests for SARS-CoV-2 antibodies do not reflect the richness and durability of immune memory to SARS-CoV-2." For the lay person to understand the results better, a definition is in order. "Memory T cells are antigen-specific T cells that remain long-term after an infection has been eliminated. The memory T cells are quickly converted into large numbers of effector T cells upon reexposure to the specific invading antigen, thus providing a rapid response to past infection." [ScienceDirect.com] Also for the lay person, from the NIH's summary of the study's results: "Several months ago, our studies showed that natural infection induced a strong response, and this study now shows that the responses last.... We are hopeful that a similar pattern of responses lasting over time will also emerge for the vaccine-induced responses."
STUDY #10: KOREAN STUDY
"Antibody Responses One Year after Mild SARS-CoV-2 Infection"
Published 5/21/2021, Journal of Korean Medical Science
https://jkms.org/DOIx.php?id=10.3346/jkms.2021.36.e157
This study shows that antibodies from natural Covid-19 infection last at least one year in 94% of test subjects. They used four commercially available and FDA-approved (for emergency use) antibody tests to conduct their testing. Will Covid-19 antibodies last two or three years? It's too early to tell, since Covid-19 hasn't been around that long. By comparison though, "in case of SARS-CoV-1 [the SARS virus from 2003], 90% and 50% of patients have been shown to maintain IgG antibodies for two and three years, respectively.... Understanding the long-term kinetics of antibodies in COVID-19 is essential in interpreting serosurvey data. We investigated the antibody response one year after infection in 52 mildly symptomatic patients with SARS-CoV-2 infection, using three commercial immunoassays and a surrogate virus neutralization test (sVNT) kit. Anti-N pan-immunoglobulin (Ig), anti-S IgG, and anti-S1 IgG were detected in 43 (82.7%), 44 (84.6%), and 30 (57.7%), respectively. In 49 (94.2%), the antibody could be detected by either anti-N pan-Ig or anti-S IgG assay. In the sVNT, 30 (57.7%) had positive neutralizing activity. Despite waning immunity, SARS-CoV-2 antibodies can be detected up to one year after infection, even in mild COVID-19 patients.... None of the patients reported exposure to other COVID-19 patients or developing symptoms of COVID-19 after recovery."
STUDY #11: WASHINGTON UNIVERSITY SCHOOL OF MEDICINE STUDY
"SARS-CoV-2 Infection Induces Long-Lived Bone Marrow Plasma Cells in Humans"
Published 5/24/2021, Nature
https://www.nature.com/articles/s41586-021-03647-4
This study was conducted by the Ellebedy Laboratory at the Washington University School of Medicine, with the purpose of determining "whether infection with SARS-CoV-2 induces antigen-specific long-lived BMPCs in humans", basically long-lasting immune memory in the bone marrow of recovered individuals. "Overall, our results indicate that mild infection with SARS-CoV-2 induces robust antigen-specific, long-lived humoral immune memory in humans." The study analyzed blood samples "from 77 individuals who were convalescing from COVID-19, the majority of whom had experienced mild illness (7.8% hospitalized)". Blood samples were collected at 3-month intervals, the last of which was 7 months after the onset of symptoms. "In addition, bone marrow aspirates were collected from 18 of the convalescent individuals at 7 to 8 months after infection." Final samples were collected from a subset of participants approximately 11 months after infection. "We detected SARS-CoV-2 S-specific BMPCs in bone marrow aspirates from 15 out of 19 convalescent individuals, and in none from the 11 control participants.... Although we detected anti-S IgG antibodies in serum [from blood samples] at least 7 months after infection in all 19 of the convalescent donors from whom we obtained bone marrow aspirates, we failed to detect S-specific BMPCs in 4 donors. Serum anti-S antibody titres in those four donors were low, suggesting that S-specific BMPCs may potentially be present at very low frequencies that are below the limit of detection of the assay." You can read a writeup and summary of the results for the lay person by the publisher here: "Had COVID? You'll probably make antibodies for a lifetime"
STUDY #12: THAI STUDY
"SARS-CoV-2 Variants of Concern Exhibit Reduced Sensitivity to Live-Virus Neutralization in Sera from CoronaVac Vaccines and Naturally Infected COVID-19 Patients"
Posted 7/15/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.07.10.21260232v2.full-text
This study compared the effectiveness of the CoronaVac vaccine against four variants of SARS-CoV-2 (Original, Alpha, Beta, and Delta) with that of natural infection from patients recovered in 2020 and patients recovered in 2021. It was all conducted in-vitro. The researchers used blood serum derived from three groups: 1. a group of 60 healthcare workers who'd received the CoronaVac vaccine (CoronaVac Group); 2. a group of 30 Covid-19 patients who'd been hospitalized in 2020 (Natural Infection 2020 Group); and 3. a group of 30 Covid-19 patients who'd been hospitalized in 2021 (Natural Infection 2021 Group). CoronaVac is a 2-dose vaccine being used for mass vaccination in China, Thailand, and various low-income countries; its efficacy is comparable to the Johnson & Johnson vaccine. In basic language, the blood serum from each participant was pitted against the four strains of virus in test tubes to see whose antibodies were effective in neutralizing the viruses. The first result is "Sera from both CoronaVac vaccines and naturally infected individuals had significantly reduced neutralizing capacity against all 3 VOCs [Variants of Concern: Alpha, Beta & Delta] compared to WT [Original strain]". Blood serum from all three groups showed neutralizing capability against the Original Wuhan strain (98% for CoronaVac, and 100% for both Natural Infection 2020 & 2021). 75% of the CoronaVac Group showed neutralizing capability against the Alpha variant compared with 97% for both Natural Infection 2020 & 2021. 70% of the CoronaVac Group showed neutralizing capability against the Beta variant compared with 93% for Natural Infection 2020 and 97% for Natural Infection 2021. 48% of the CoronaVac Group showed neutralizing capability against the Delta variant compared with 87% for Natural Infection 2020 and 93% for Natural Infection 2021. "These results are consistent with the predominant strains that circulated in Thailand in early/mid-2020 and mid-2021 at the time of sample collection.... Our study highlights a low degree of neutralization-afforded protection mounted by CoronaVac when compared to natural infection."
STUDY #13: PUBLIC HEALTH ENGLAND STUDY
"Effectiveness of COVID-19 vaccines against the B.1.617.2 variant"
Posted 5/24/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.05.22.21257658v1.full-text
This study measured the efficacy of the 2-dose Pfizer and 2-dose AstraZeneca vaccines against the Alpha and Delta variants. In preventing symptomatic Covid-19, the Pfizer vaccine had 93% efficacy against the Alpha variant and 88% against the Delta variant, while the AstraZeneca vaccine had 66% efficacy against the Alpha variant and 60% efficacy against the Delta variant. In preventing hospitalization and death, the efficacy of both vaccines was even higher. Though the Delta variant reduced the efficacy of both vaccines by 5%-6%, both vaccines were still quite effective against the Delta variant.
STUDY #14: CDC KENTUCKY STUDY
"Reduced Risk of Reinfection with SARS-CoV-2 After COVID-19 Vaccination — Kentucky, May-June 2021"
Posted 8/6/2021, CDC MMWR Early Release
https://www.cdc.gov/mmwr/volumes/70/wr/mm7032e1.htm
This retrospective study followed two groups of individuals who all tested positive for Covid-19 in 2020. Remember that fact: Every person in both groups tested positive for Covid-19 in 2020. Group #1, the Test Group, consisted of everyone — 246 people total — who tested positive again in May or June of 2021. Group #2, the Control Group, was a 2:1 matching group of 492 randomly selected people who did not receive a subsequent positive test result by the end of June 2021. So Group #2 consisted of people who did not test positive again in 2021 by the June 30th cutoff date. No 2021 Covid-19 test was required for the Control Group, meaning that many in the Control Group did not actually get tested in May or June of 2021. So this study assumes that all of the Control Group's test results would have come back negative if they had been tested in May or June of 2021. The study looked at the number of people in each group that were fully vaccinated, finding that 20% of Group #1 were fully vaccinated versus 34% of Group #2. Based on this, they concluded that unvaccinated people were more than twice as likely as vaccinated people to acquire their second Covid-19 infection. The study issues the following recommendation: "To reduce their likelihood for future infection, all eligible persons should be offered COVID-19 vaccine, even those with previous SARS-CoV-2 infection." But this recommendation is a logical fallacy. To gain the same level of protection, vaccinated people would have to go out and actively seek Covid-19 infection. Imagine if the CDC had also recommended the following: To reduce their likelihood for future infection, all vaccinated persons should be offered an injection of live COVID-19 virus.
Recall that this study only follows people who had positive Covid-19 tests. Therefore, it has nothing to say about the benefits of vaccination-only versus the benefits of natural-immunity-only. Vaccination, by itself, is considered excellent protection by the CDC and as shown by other studies. Natural infection, by itself, is also considered excellent protection as shown by other studies. So the actual question raised by this study is: Does the combination of natural infection and vaccination provide a level of super-protection? ...a level of protection beyond that provided by vaccination alone or natural immunity alone? The study concludes that it does. But before you get too excited about that prospect, let's take a deeper look at the study.
You may have already noticed the fatal flaw in this study. In any statistical study that compares two groups, it's critical to treat both groups using the same standards. Control Group #2 was not subject to the same testing requirements as Test Group #1. ALL of Group #1 got retested in May or June of 2021. We don't know how many, if any, of Group #2 got retested in May or June of 2021. If the entire Control Group had been retested, as standards would dictate, it's likely that some of them would have tested positive, which means they should have instead been part of Group #1. So Group #2 likely contained people that should have actually been in Group #1. The study itself acknowledges a similar limitation: "Persons who have been vaccinated are possibly less likely to get tested. Therefore, the association of reinfection and lack of vaccination might be overestimated." Best practice would be to rerun the study and only include people in Group #2 who tested positive in 2020, who did not subsequently test positive in January-June 2021, and who tested negative in May/June 2021. It's possible that subjects who meet these three criteria might be insufficient in numbers to conduct a proper study.
A third problem with this study, a potential source of bias, is the random matching of controls to test subjects. Any bias or error in the randomization algorithm could result in something akin to a stacked deck of cards. Better practice would be to run the experiment not once but dozens or hundreds of times, each time randomly selecting a different Control Group. Best practice would be to not randomly select at all, but to expand the Control Group to all eligible subjects. This brings up the question, Why Kentucky? What about the other 49 states? Could this whole study be just an exercise in data mining? ...aka cherry picking your state to provide the desired results? The authors should rerun the study using data from all 50 states and correct at least the one fatal flaw. If the results were to turn out the same using a large data set, that would provide strong evidence that the combination of vaccine and natural infection is super-protective. To their credit, the study authors acknowledge the following: "This is a retrospective study design using data from a single state during a 2-month period; therefore, these findings cannot be used to infer causation. Additional prospective studies with larger populations are warranted to support these findings."
A fourth limitation, noted in the study, is the possibility that some positive test results in May/June 2021 were not actual reinfections but detections of the original infection.
A fifth issue in this study is that it relies exclusively on Covid-19 "NAAT or antigen test results", without confirmation by symptoms. So the study includes asymptomatic people and false positives in both groups. Both groups are supposed to consist only of people with natural immunity. As we discussed before (see Question #13 above), it's uncertain whether someone who merely tests positive for Covid-19, without accompanying symptoms, should be considered naturally immune. It would be interesting to see what the results would be if only symptomatic cases were counted as positive. Compounding the bias, Group #1 was tested twice to determine initial infection in 2020 and subsequent reinfection in 2021, doubling the possibility of false positives and asymptomatic test results for this group. We don't know how many people would have been excluded from Group #1 if accompanying symptoms had been required on both the front-end test and the back-end test, but it's likely a large percentage of the group would have been dropped from results.
It's worth mentioning that this CDC study is not like the others. First of all, it's incomplete. The CDC thought the results were so important that they rushed out this early release, pre-publication. The full data set is not made available for outside scrutiny. Though the study fails to meet basic scientific standards, we peer review it nevertheless, as if it had been submitted to a journal for publication. Normally, such a study wouldn't qualify for inclusion with the others, but apparently this one is very important. The CDC, primarily based upon this study, is recommending that the naturally immune get vaccinated, a logical fallacy that does not follow from the results of the study. Much of the US media is also citing this study without giving it critical review.
There's a standard disclaimer that accompanies all unpublished and pre-published work on the MedRxiv Preprint Server: "This article is a preprint and has not been peer-reviewed. It reports new medical research that has yet to be evaluated and so should not be used to guide clinical practice." This disclaimer should more-so apply to any self-published reports by the CDC, such as this Kentucky study, that have not been the subject of outside scientific scrutiny by peers. We say "more-so" because the MedRxiv Server includes an active comments section where researchers can get preliminary feedback and review from scientists and the general public. CDC reports, on the other hand, are not peer reviewed, are not tagged by the much-needed disclaimer, and do not have a comments section for scientists to provide feedback. Just because they're unpublished or pre-published does not make scientific works invalid. Most of them will eventually be published. They just need to be scrutinized carefully, as we've done in this article, before their results are accepted.
Let's apply a plausibility test to the CDC Kentucky Study. This study is asking us to believe that 246 people in Kentucky got Covid-19 in 2020, then recovered, then 67 of them got vaccinated, and then all of them got Covid-19 again in 2021. This would indeed be a surprising result, highly newsworthy. With recurrence of Covid-19 being so rare, individuals who get the disease twice often become the subject of news stories. We conducted an internet search looking for confirmation and examined the top 100 Google search results for "Kentucky Man Gets Covid Twice" and the top 100 for "Kentucky Woman Gets Covid Twice" (without the quotes each time) looking for anyone who might have been part of this CDC Kentucky Study. The 200 search results yielded a large percentage of links back to and news stories about the CDC Kentucky Study. They yielded news stories about the Hong Kong man who got Covid-19 twice. Our search yielded three potentially relevant news stories. The first was about a Kentucky man who had had Covid-19 twice, but both cases were in 2020, so he was not part of this CDC Kentucky Study. The second story was a CDC article about an outbreak of two reinfections in a Kentucky nursing home. However, both of these reinfections also occurred in 2020, so were not part of this CDC Kentucky Study. The final result yielded one person who was actually part of this study! "Louisville woman gets COVID again after being fully vaccinated". The woman tested positive for Covid-19 in November 2020, got vaccinated in April 2021, then tested positive again in May/June 2021, making her part of Group #1. When she tested positive in November 2020, she was asymptomatic. In June 2021, she had moderate symptoms and was sick for several days.
Through an internet search we found no evidence of a rampant outbreak of reinfections in Kentucky. We found a single 1 out of 246 study participants in Group #1, who had no symptoms when tested in 2020, meaning she was either asymptomatic or a false positive. She would not have been included in this study if a symptomatic requirement had been implemented. What about the other 245 people? Will some, most, or all of them drop out of Group #1 if we implement a symptomatic requirement on both the first and second tests? Most certainly, but we can't know the exact percentage who will drop out without having data on their symptoms.
The CDC Kentucky Study states: "Few real-world epidemiologic studies exist to support the benefit of vaccination for previously infected persons." It looks like the CDC didn't find any such studies, and the only such study we found was this CDC Kentucky Study. So the CDC is relying entirely on this small, fatally flawed, Kentucky study to provide real-world evidence. On the other hand, many large-scale, real-world studies do exist that show natural immunity is indeed powerful protection. It's troubling that the CDC does not cite nor acknowledge the existence of any of these prior natural immunity studies, including the Siren Study [#4], the Cleveland Clinic Study [#5], the Qatar Study [#6], the Curative Study [#7], the Denmark Study [#8], and the Israeli Study [#15]. They don't even cite Study #9 which was funded by the USA's National Institutes of Health (NIH). It's poor scientific practice to predetermine your conclusions before conducting your experiments. It's poorer practice still to deny the existence of studies that contradict your preconceived conclusions. Recommendation: Cite these other studies and stop trying to prove a point. Undertaking a study with a predetermined conclusion in mind, and ignoring all evidence to the contrary, is politics, not science.
In conclusion, we find that the CDC Kentucky Study is more politics than science, akin to the tobacco industry's studies from years past denying that cigarette smoking causes cancer. The CDC Kentucky Study tries to support a preconceived conclusion using a real-world study, while at the same time denying the existence of numerous real-world studies that support the opposite conclusion. The CDC Kentucky Study has major and fatal flaws, outlined above, that must be corrected before any conclusions can be drawn. The first flaw is the application of two Covid-19 tests to Group #1 but only one test to Group #2. The second flaw is that asymptomatic cases should ideally be excluded on both the front-end and the back-end Covid-19 tests. Excluding asymptomatic cases will also virtually eliminate false positives. The third flaw is randomly selecting subjects for Group #2; it would be better to include all eligible subjects in Group #2. The study should be expanded from one state to all 50 states. Finally, if the study were to be conducted properly and the results were to turn out the same, the CDC should correct the logical fallacy in their recommendation. The study's results don't actually support the recommendation that naturally immune people get vaccinated; they only support the premise that naturally immune people can gain additional protection through vaccination. To set national vaccine policy based upon this fatally flawed and inconclusive study, when the preponderance of scientific evidence suggests otherwise, is irresponsible.
STUDY #15: ISRAELI STUDY
"Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel"
Posted 4/20/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.04.20.21255670v1.full-text
This large-scale study was conducted using the entire population of Israel as participants. It looked at the efficacy of the Pfizer Vaccine and that of Natural Immunity with respect to preventing four outcomes: "documented infection" (using PCR tests), severe illness, hospitalization, and death. "Data on symptoms were also available but we found them less reliable and thus did not include symptomatic COVID-19 as an outcome." Follow-up duration was three months and, during the time of the study, Alpha "was by far the most prevalent variant".
"Vaccination was highly effective with overall estimated efficacy for documented infection of 93%; hospitalization 94%; severe illness 94%; and death 94%. Similarly, the overall estimated level of protection from prior SARS-CoV-2 infection for documented infection is 95%; hospitalization 94%; and severe illness 96%.... As there were only 1 death cases in the Recovered Cohort [group consisting of 187,000+ people], protection against death was not estimated.... Our results question the need to vaccinate previously-infected individuals."
Compared to other large-scale population studies, the Israeli Study is much larger. "These two [prior] studies are based on 11,727 [Denmark Study #8] and 6,614 [Siren Study #4] previously infected individuals, with 72 and 44 reinfections, respectively. In comparison, the Recovered cohort in our study comprised 187,549 individuals, with 894 reinfections."
Notably, the Israeli Study contradicts the Denmark Study's finding of sharply lower efficacy for individuals aged 65+. Israeli Study: "Vaccine efficacy was quite similar in all age groups with some decrease in efficacy [1%-7% decrease] for the 80+ age category." Likewise, natural-immunity-efficacy was similar across all age groups with only a 0%-3% decline for ages 80+.
STUDY #16: DELTA STUDY (ISRAEL)
"Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections"
Posted 8/25/2021, MedRxiv Preprint Server for Health Sciences
https://www.medrxiv.org/content/10.1101/2021.08.24.21262415v1.full
This most recent study, also out of Israel, is concerned entirely with the Delta variant. "This study demonstrated that natural immunity confers longer lasting and stronger protection against infection, symptomatic disease and hospitalization caused by the Delta variant of SARS-CoV-2, compared to the BNT162b2 [Pfizer] two-dose vaccine-induced immunity.... This is the largest real-world observational study comparing natural immunity, gained through previous SARS-CoV-2 infection, to vaccine-induced immunity." Over 750,000 people were eligible for inclusion in the various groups. It compared three groups, a Vaccination Group, a Natural Immunity Group, and a Hybrid Immunity Group. It did not include a fourth "No Immunity" group, presumably because unvaccinated people with no prior infection were in short supply.
Group #1: Vaccination Group (No Natural Immunity or Boosters): People who received two doses of Pfizer Vaccine before March 2021. These people did NOT have a positive PCR test result by 6/1/2021 (no natural immunity) and didn't receive a third booster dose by the end of the follow-up period (no booster).
Group #2: Natural Immunity Group (No Vaccination): Previously infected people determined by a positive PCR test anytime before March 2021, and who had not been vaccinated by the end of the follow-up period.
Group #3: Hybrid Immunity Group (Natural Immunity + Vaccination): Previously infected people determined by a positive PCR test anytime before March 2021, and who received a single booster dose of vaccine by 5/25/2021 (7 or more days before the follow-up period). Israeli Ministry of Health guidelines allow previously infected individuals "to receive one dose of the vaccine, after a minimum 3-month-interval from the date of infection."
The Pfizer Vaccine was used for all vaccinations in this study. "Outcomes were evaluated during the follow-up period of June 1 to August 14, 2021, ...corresponding to the time in which the Delta variant became dominant in Israel.... The Delta variant...has been the dominant strain in Israel since June 2021." Three models were run, explained below, to compare outcomes among the three groups.
Model #1: Vaccination Group #1 vs Natural Immunity Group #2 (with Time Matching) — "These two groups were matched in a 1:1 ratio by age, sex, GSA [geographic area] and time of first event. The first event was either the time of administration of the second dose of the vaccine or the time of documented infection with SARS-CoV-2 (a positive PCR test result), both occurring between January 1, 2021 and February 28, 2021.... We matched 16,215 persons in each group.... During the follow-up period, 257 cases of SARS-CoV-2 infection were recorded, of which 238 occurred in the vaccinated group (breakthrough infections) and 19 in the previously infected group (reinfections). After adjusting for comorbidities, we found a statistically significant 13-fold increased risk for breakthrough infection as opposed to reinfection.... For symptomatic SARS-COV-2 infections during the follow-up period, 199 cases were recorded, 191 of which were in the vaccinated group and 8 in the previously infected group. After adjusting for comorbidities, we found a 27-fold risk for symptomatic breakthrough infection as opposed to symptomatic reinfection.... Nine cases of COVID-19-related hospitalizations were recorded, 8 of which were in the vaccinated group and 1 in the previously infected group. No COVID-19-related deaths were recorded in our cohorts."
Model #2: Vaccination Group #1 vs Natural Immunity Group #2 (No Time Matching) — "Matching was done in a 1:1 ratio based on age, sex and GSA alone.... We matched 46,035 persons in each group." The average time of event favors vaccination in this model. All vaccinations were performed in January or February 2021, while prior infections went all the way back to March 2020 with most them happening in or near September 2020. Hence the age of antibodies in this model is stacked an average of several months in favor of vaccination. During "the follow-up period, 748 cases of SARS-CoV-2 infection were recorded, 640 of which were in the vaccinated group (breakthrough infections) and 108 in the previously infected group (reinfections). After adjusting for comorbidities, a 6-fold increased risk for breakthrough infection as opposed to reinfection could be observed.... 552 symptomatic cases of SARS-CoV-2 were recorded, 484 in the vaccinated group and 68 in the previously infected group. There was a 7-fold increased risk for symptomatic breakthrough infection than symptomatic reinfection. COVID-19 related hospitalizations occurred in 4 and 21 of the reinfection and breakthrough infection groups, respectively.... No COVID-19-related deaths were recorded.... Although the results could suggest waning natural immunity against the Delta variant, those vaccinated are still at a 6-fold increased risk for breakthrough infection and at a 7-fold increased risk for symptomatic disease compared to those previously infected. SARS-CoV-2-naive vaccinees were also at a greater risk for COVID-19-related-hospitalization compared to those who were previously infected."
Model #3: Natural Immunity Group #2 vs Hybrid Immunity Group #3 (No Time Matching) — Model #3 asks the question: Does vaccination provide any additional benefit in previously infected individuals? The model matched 14,029 people in each group. The numbers are so small that it's hard to draw any conclusions. The only statistically significant result included asymptomatic cases: "We found that the latter group [Hybrid Immunity] had a significant 0.53-fold (95% CI, 0.30 to 0.92) decreased risk for reinfection, as 20 had a positive RT-PCR test, compared to 37 in the [Natural Immunity Group].... Symptomatic disease was present in 16 single dose vaccinees and in 23 of their unvaccinated counterparts. One COVID-19-related hospitalization occurred in the unvaccinated previously infected group. No COVID-19-related mortality was recorded." Note that the Hybrid Immunity Group contained people (19% of them) who had been vaccinated then subsequently infected. When the model was restricted to only those who had been infected and subsequently vaccinated (81% of them), statistical significance could no longer be demonstrated. The order of events is important for naturally immune people who are considering vaccination and also for vaccinated people who want to know their immunity status should they become infected with the virus. The authors conclude that "Individuals who were previously infected with SARS-CoV-2 seem to gain additional protection from a subsequent single-dose vaccine regimen.... [However], we could not demonstrate significance in our cohort."
A very significant and practical conclusion can be reached if we combine the results from all three models. This conclusion is of great interest to vaccinated people. The conclusion is that vaccinated people can gain the highest level of immunity, immunity equal to or greater than that of naturally immune people, simply via environmental exposure to the virus. The risk from exposure is minimal, though not absolutely zero. A practical conclusion is that most vaccinated people can go about their everyday lives as normal, even mask-free, without worrying about possible exposure to the virus. This conclusion is equally applicable to most naturally immune people who already enjoy the highest level of protection.
Why does natural immunity beat vaccine-induced immunity? We can only speculate. Vaccination has always served as a substitute for actual infection. Yet it's hard to match, much less beat, the protective effects of the real thing. The authors speculate that natural immunity might provide a "more extensive immune response to the SARS-CoV-2 proteins than that generated by the anti-spike protein immune activation conferred by the vaccine". Another possibility is the method of delivery: oral/nasal entry for natural infection versus muscular injection for vaccination. It's well known that the mucosal immune system provides a first line of defense and that many vaccines provide incomplete mucosal immunity. Hence, naturally immune people may possess a first line of defense lacking in vaccine-injected people.
We don't know how a truly unvaccinated / no prior immunity control group would have performed during this time period, but we can make a ballpark estimate using another study, and we can express the results in terms of our favorite measure, efficacy. The Public Health England Study shows that the Pfizer vaccine has 88% efficacy in preventing symptomatic Covid-19 caused by the Delta variant. Using Model #1, an 88% reduction in risk translates into a 9.8% infection rate in our hypothetical control group, meaning 1592 people would have developed a symptomatic breakthrough infection in our hypothetical "No Immunity Group". In Model #1, if we assign the Vaccinated Group an 88% efficacy rating, then the Natural Immunity Group would have a 99.5% efficacy rating.
Original (Wuhan, China) Wuhan-Hu-1
Alpha (Great Britain) B.1.1.7
Beta (South Africa) B.1.351
Gamma (Brazil) P.1
Delta (India) B.1.617.2
Epsilon (California, USA) B.1.427 & B.1.429
Zeta (Brazil) P.2
Eta (Multiple Countries) B.1.525
Theta (Philippines) P.3
Iota (New York, USA) B.1.526
Kappa (India) B.1.617.1
Lambda (Peru) C.37
Mu (Colombia) B.1.621
BNT162b2 is the 2-Dose Pfizer-BioNTech Vaccine
mRNA-1273 is the 2-Dose Moderna Vaccine
Ad26.COV2.S is the 1-Dose Johnson & Johnson Vaccine
ChAdOx1 is the 2-Dose AstraZeneca vaccine
SARS-CoV-2 is the virus causing COVID-19, so named because of its similarity to the original SARS virus from 2003 known as "SARS-CoV" or "SARS-CoV-1".
If you'd like to conduct your own research on the latest scientific studies regarding Covid-19, a good place to start is the searchable database maintained by the World Health Organization, COVID-19: Global Literature on Coronavirus Disease, which contains over 350,000 studies from across the world. Another excellent database is the MedRxiv Preprint Server for Health Sciences which contains pre-publication versions of the most recent medical research.
→ Duration of Humoral Immunity to Common Viral and Vaccine Antigens
→ Not Just Antibodies: B Cells and T Cells Mediate Immunity to COVID-19
→ Mucosal Immunity in COVID-19: A Neglected but Critical Aspect of SARS-CoV-2 Infection
→ SARS-CoV-2-specific T Cell Immunity in Cases of COVID-19 and SARS, and Uninfected Controls
→ Duration of Humoral Immunity to Common Viral and Vaccine Antigens
→ Considerations in Boosting COVID-19 Vaccine Immune Responses
→ Repeated Exposure to Subinfectious Doses of SARS-CoV-2 May Promote T Cell Immunity and Protection against Severe COVID-19
→ Antibodies Elicited by mRNA-1273 Vaccination Bind More Broadly to the Receptor Binding Domain than Do Those from SARS-CoV-2 Infection
→ SARS-CoV-2 Seropositivity and Subsequent Infection Risk in Healthy Young Adults: A Prospective Cohort Study
→ Lasting Immunity Found After Recovery from COVID-19
→ Had COVID? You'll probably Make Antibodies for a Lifetime
About the Author — The author has published and peer-reviewed numerous papers for scientific journals, books, and conference proceedings. He holds three degrees in mathematics and computer science, including a PhD from the University of Illinois, where he specialized in genetic algorithms, complex systems, statistical methods, artificial intelligence, and machine learning, and was part of the research team for the Illinois Genetic Algorithms Laboratory. He's worked for companies both big and small. After "retiring" from the corporate world over 20 years ago, he's worked only for himself, those around him, and the benefit of society in general.
Funding / Interests — No funding was sought or received for this research. No conflicts of interest exist.
© Copyright Notice — This article is copyright 2021 by the author with all rights reserved. Permission is granted to share and quote all or part of this writing, as long as proper attribution is made and a link back to this original article is made. Please link back to the following address — www.USABottomLine.com/1/